The traditional fee-for-service healthcare system has been failing patients, providers, and payers for decades. From skyrocketing costs, to 15-minute visits with harried doctors rushing from patient to patient, to fragmented care and poor clinical outcomes, healthcare offers a plethora of challenges we must overcome in our efforts to achieve the elusive quadruple aim: better outcomes, at a lower cost, with improved patient and provider experiences.
Accountable Care Organizations (ACOs) stand at the forefront of efforts to overcome these challenges and transform patient care.
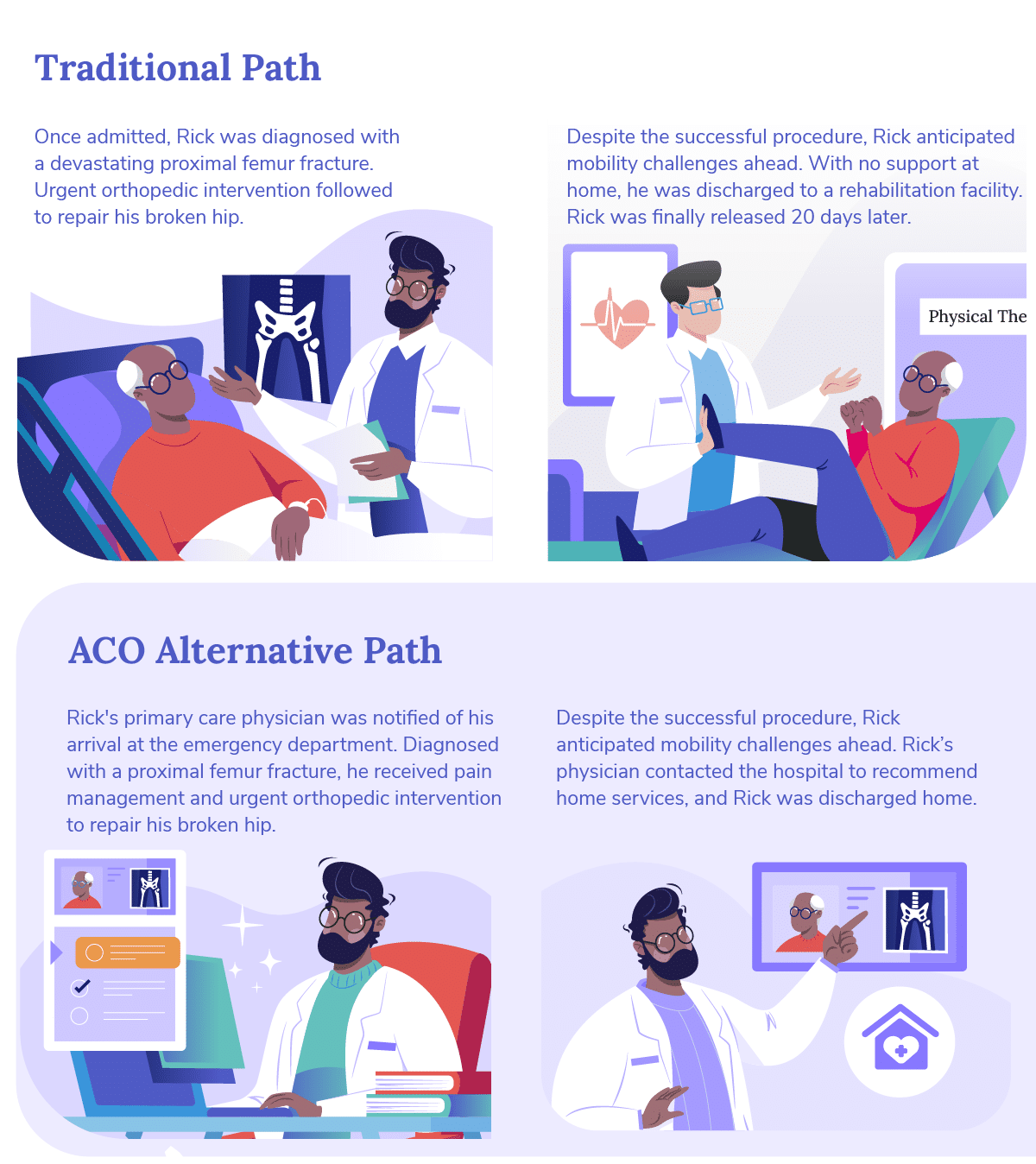

As highlighted above, ACOs like Pearl are reshaping healthcare delivery, emphasizing value over volume, and care coordination over fragmentation. In addition to improving patient care during acute episodes like Rick’s by better addressing social determinants of health and redirecting resources toward earlier stages of care, ACOs are aligning the healthcare experience with patient preferences, while also improving long-term health outcomes.
Join us on this exploration of the multifaceted approach ACOs take to enable value-based care (VBC), where innovation meets compassion in service of a better system.
How ACOs Ensure Accurate Benchmarking
Risk, on an individual and population level, is a cornerstone in the foundation of VBC; accurate and continually-updated benchmarking equips practices for success in nearly all delivery models. For those who are new to value-based care, the benchmark is the payer-established budget unique to each ACO based on the disease burden, regional cost of care, historic care utilization, and proportion of underserved beneficiaries in a given population. Organizations participating in VBC programs must manage their attributed patients within — and ideally far below — this budget while maintaining or improving care quality for the duration of the performance year.
ACOs have invested substantial capital and research into appropriate benchmarking, and equip their participating providers with the tools and insights needed to preemptively avoid common gaps in risk. As an example, CMS’ Hierarchical Categorization Coding (HCC), which is used to determine individual benchmarks for Medicare, relies on non-intuitive clinical actions: for example, annually re-diagnosing chronic conditions. By leveraging technology, ACOs are able to nurture more accurate benchmarks, resulting in performance margins. By leveraging data, ACOs can scrutinize the entire healthcare delivery landscape to pinpoint opportunities for better outcomes at the same or lower costs.
This data-driven approach enables ACOs to make informed decisions and allocate resources more efficiently. For example, the data has shown us that one of the most effective ways to reduce risk is to maintain regular touchpoints with patients through preventive care activities like Annual Wellness Visits (AWVs). Regular AWVs are associated with better patient outcomes, as they provide an opportunity for early detection and intervention,1 and so Pearl has invested in helping providers identify and act on patients eligible for AWVs.
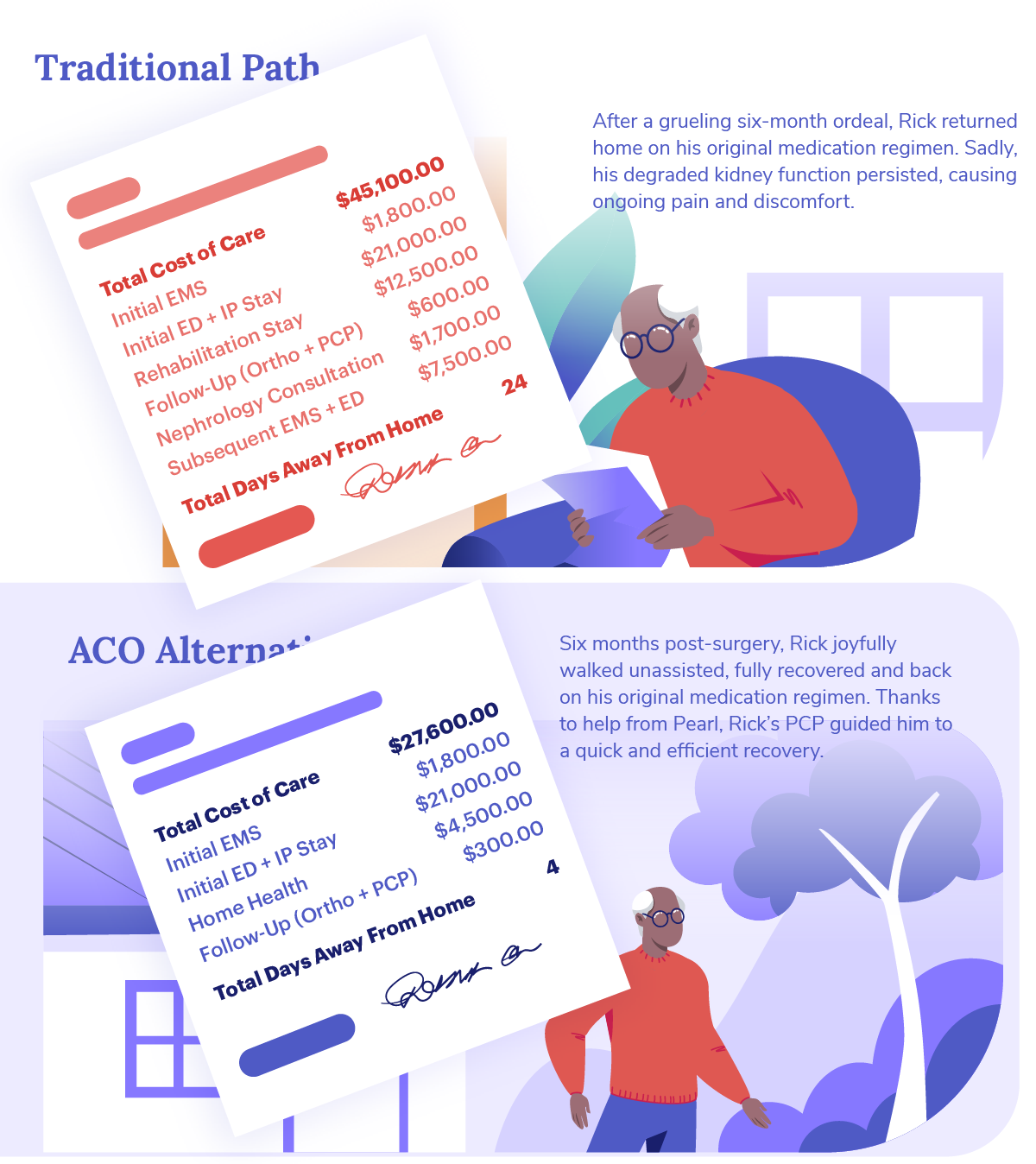
Eliminating Fragmentation
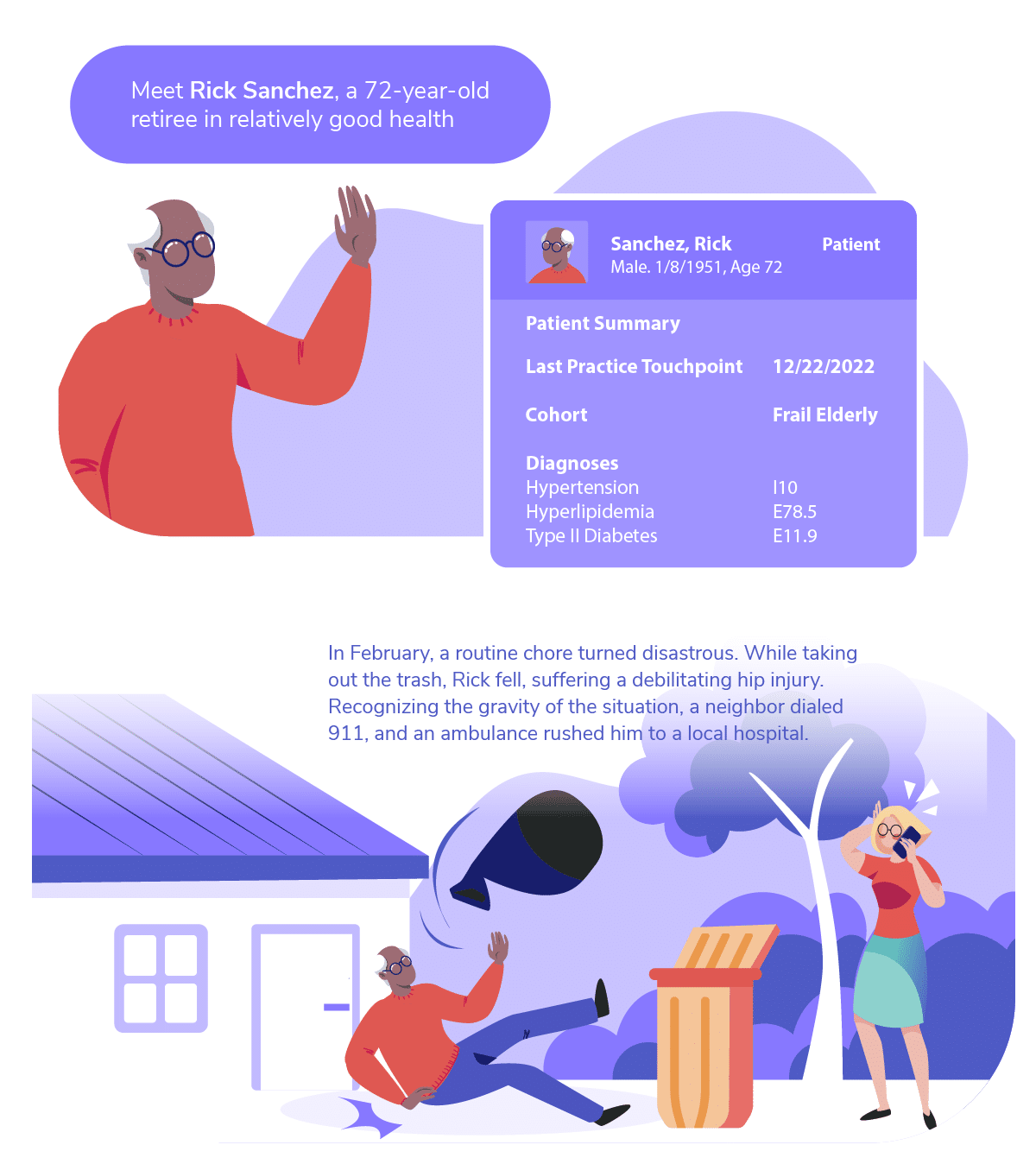
Fragmented care has long been deterimental to outcomes, and it has become increasingly problematic given the interoperability challenges presented by digital care delivery. Poorly coordinated care leads to reduced quality of care, poor patient experiences, wasted resources, duplicative diagnostics, and worst of all, medical errors.2 Many ACOs are taking significant steps to reduce fragmentation by fostering interoperability and data sharing. For example, as Rick’s story showed, Pearl Health serves as the bridge that connects disparate sources of information, making it far likelier that a patients’ care continues to progress efficiently, even when transitions of care (e.g., hospital discharge) present barriers.
More comorbid populations make this challenge even more complex, with most Medicare beneficiaries having, on average, more than a dozen individual contact points in a given year.3 A given PCP’s patient panel will often be co-managed by more than 100 different specialist providers.4 When patients move between various healthcare settings, such as hospitals-to-home or skilled-nursing-facilities-to-hospices, information is frequently lost due to technical challenges and disparate systems. Because ACOs rely on the downstream economics, garnered by efficient care, they are likely to make substantial investments in information systems, leveraging the promise of interoperable data by creating a single narrative from the patchwork of poorly integrated systems.
Harnessing Data Science to Reduce Chaotic Care
Data science plays a pivotal role in ACOs’ mission to reduce the impact of unanticipated, chaotic care. Existing population health insights, often collated by private third-party payors, are inherently retrospective. Collectively, we wait for pathology to occur, cause symptoms (or be detected via screening), and result in a diagnosis. Only then, do providers receive gap-closure insights. With existing population health insights, care is most often reactive and focused on addressing narrow needs rather than the patient’s overall health.
As an example, consider diabetes control: the system prefers a process metric (A1c control) rather than the outcome (avoiding disabling and costly complications), or, even better, preventing diabetes from occurring in the first place. A1c control can help patients manage diabetes, but its impact is limited to that narrow scope. In comparison, because ACOs often participate in alternative payment models (APMs), they are more interested in avoiding index pathology altogether. By investing in the behaviors that make diabetes less likely to ever occur, the aggregate health of the population is improved, and the overall cost of care is reduced.
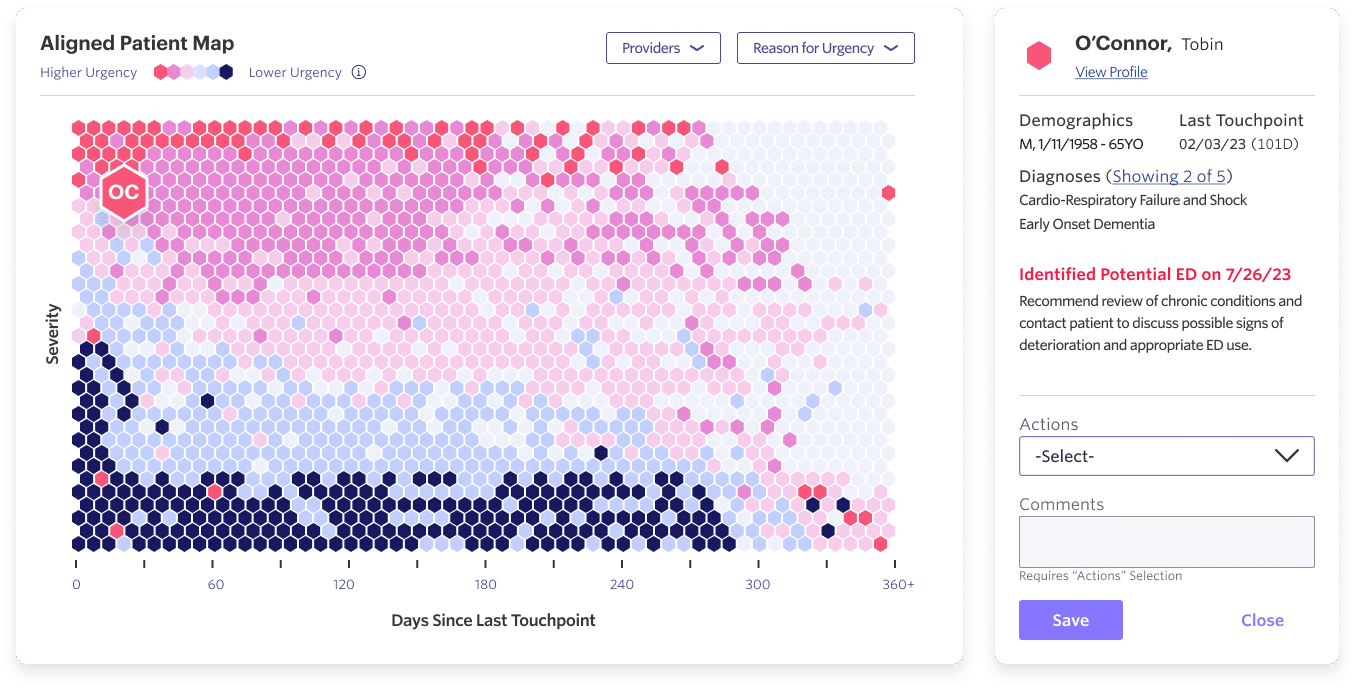
At Pearl, we are also keen to bring the promise of predictive analytics and machine learning to the bedside. By leveraging advanced analytics and predictive modeling, we can identify patients at risk of emergency department (ED) visits and equip our partner practices to proactively intervene to prevent them. This approach goes beyond the traditional taxonomy of preventable care, which tends to be symptom based, challenging established definitions and uncovering new opportunities for prevention with access to the right information.
Investing in Horizontals
A transformative aspect of accountable care is the shift from focusing solely on treating the sick to investing in prevention, including the non-clinical domains that drive population health. Traditionally, healthcare funds have been predominantly allocated to addressing existing illnesses. However, with the move from volatile and volume-driven fee-for-service to predictable value-based care payments that reward outcomes, ACOs can invest in preventing illness and promoting overall wellness. This includes addressing critical social determinants of health, such as nutrition, transportation, and access to prescription medications.
More than 20% of Medicare resources, a staggering amount, are spent during the final year of a patient’s life.5 Accountable care models enable these resources to be redirected toward healthcare at earlier stages, aligning with patients’ preferences and improving long-term health outcomes. Our own internal analysis, has corroborated the same pattern observed by others6 — well-timed proactive advanced care planning (ACP), is clearly associated with superior clinical outcomes (controlling for disease characteristics) at a lower cost.
Looking Ahead: Healthcare in 2030
While the promises of VBC have been challenged by the realities of a complicated healthcare delivery system, ACOs have led substantial progress to date, and we anticipate increasingly rapid change over the next decade.
By 2030, ACOs will likely be able to muster an entire system of value-aligned care. Consider, once again, Mr. Sanchez.
In 2030, his fall may have been avoided because in-home monitoring discovered changes to his activity and gait in the days preceding the fall. His PCP reached-out, and learned that Rick had been having trouble with his shoes. It may sound simple, but something as straightforward as replacement sneakers could have headed-off six months of suffering.
Even if a hip fracture did occur, a well-equipped ACO would help Rick to access the right care, using a constellation of the above tactics. Rick is diagnosed with the fracture, he undergoes a same-day repair, and he is discharged back to his home. Follow-up occurs in Rick’s home, via telehealth and mobile care teams. His medications are delivered, free of charge, and all diagnostics are routed back into a central platform that informs downstream predictions. The net result: one day in the hospital and tens of thousands of dollars saved.
The future of healthcare in the age of accountable care is characterized by data-driven decision-making, reduced fragmentation, targeted prevention, and improved transitions of care. ACOs like Pearl are at the forefront of this transformation, working tirelessly to provide better care at lower costs while enhancing patient experiences. As these organizations continue to evolve and innovate, the healthcare landscape will become increasingly patient-centered, efficient, and effective.
Our Technology
Beckman, A. L., & Becerra, A. Z, et al. “Medicare Annual Wellness Visit Association with Healthcare Quality and costs,” AJMC. March, 2019.
- Valenzano, C. S. “New studies reveal that fragmented care persists despite efforts to improve primary care and care delivery.” Mathematica. February, 2023.
- Internal analysis of the Pearl population.
- Barnett M.L., Bitton A., et al. “Trends in Outpatient Care for Medicare Beneficiaries and Implications for Primary Care, 2000 to 2019.” Ann Intern Med. December, 2021.
- Duncan I., Ahmed T., et al. “Medicare Cost at End of Life.” Am J Hosp Palliat Care.” March, 2019.
- Broome T., Rubin I. “End-of-Life Values and Value-Based Care.” Am J AC. May, 2022.